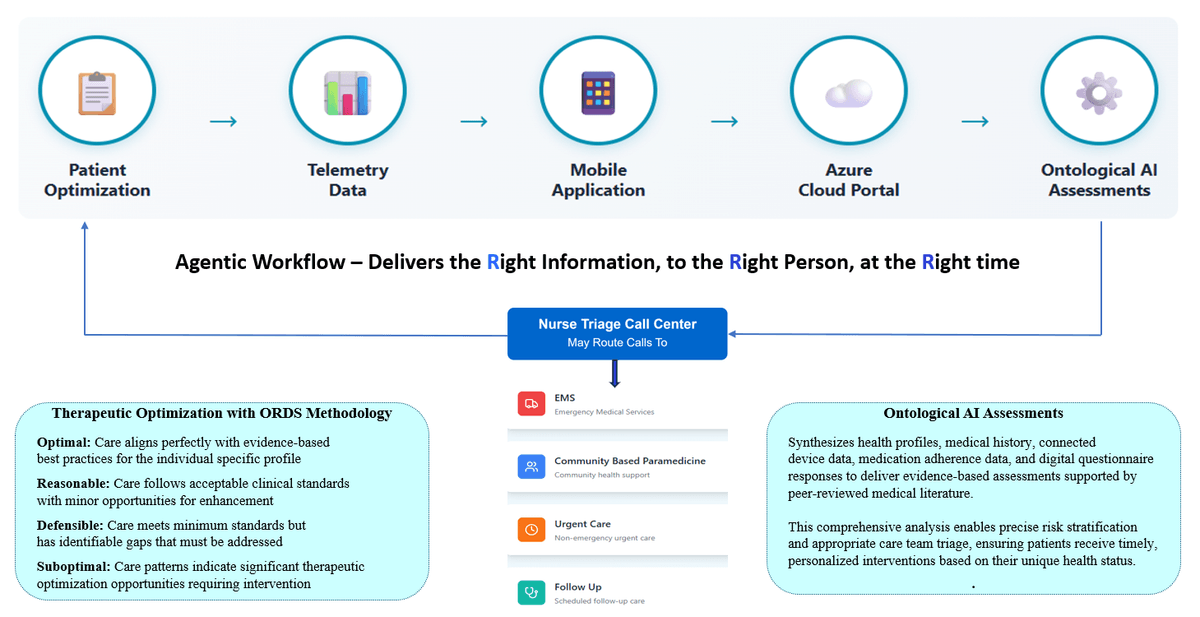
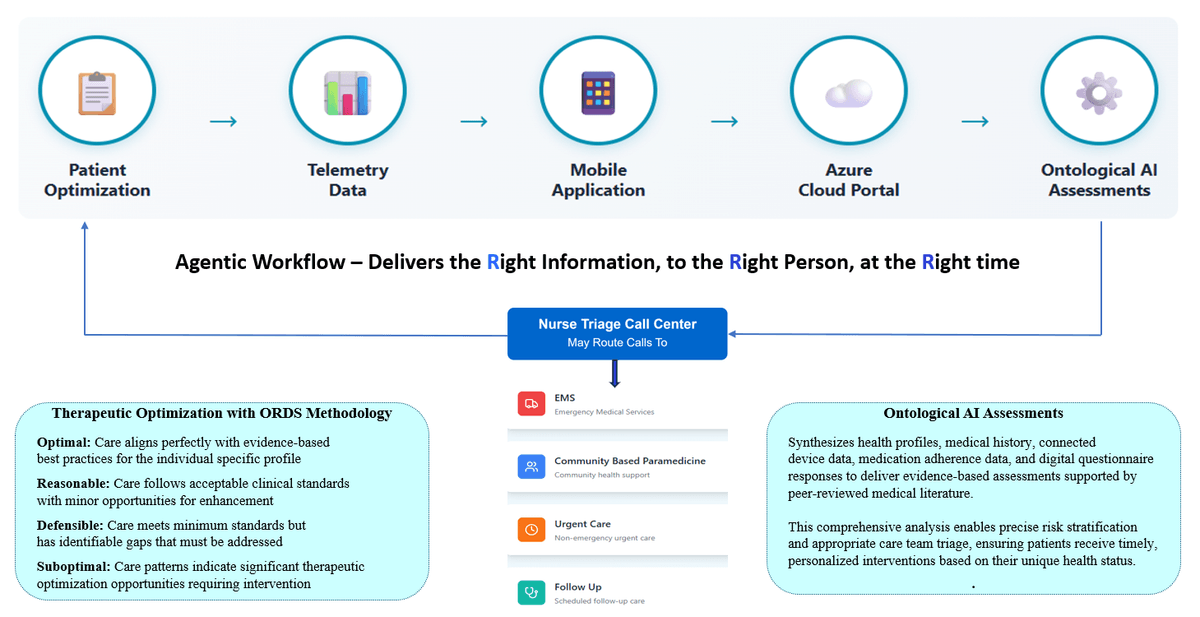
RPM/CCM - Agentic AI Workflow
Bluetooth Connected Devices
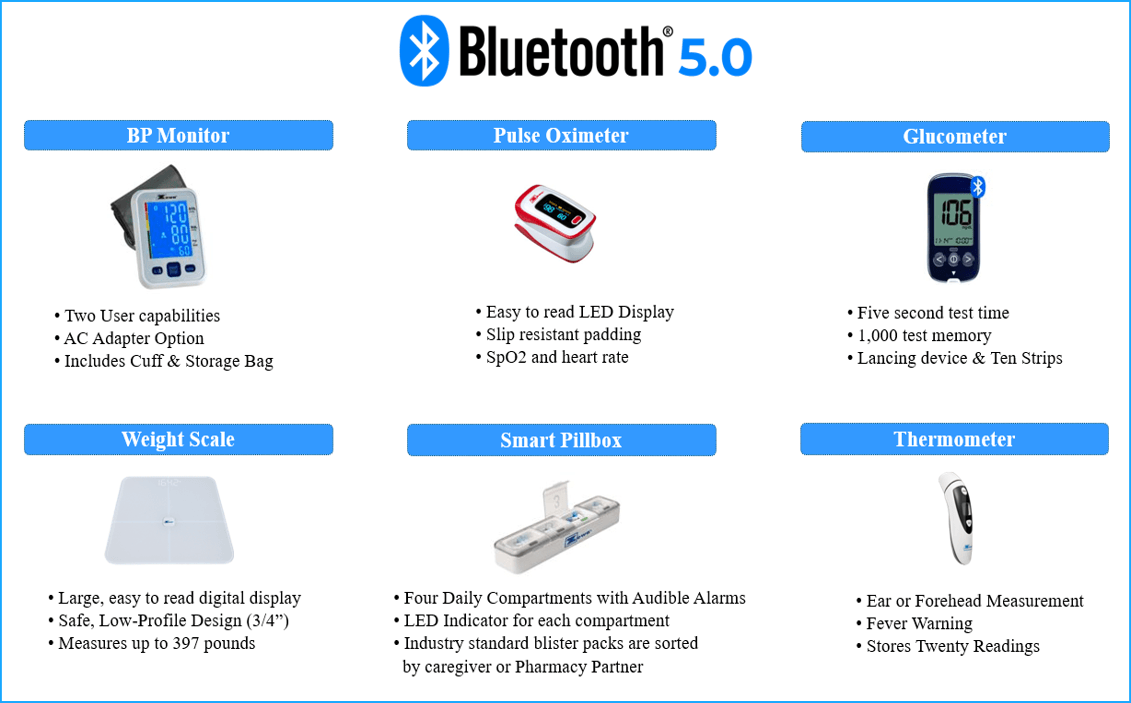
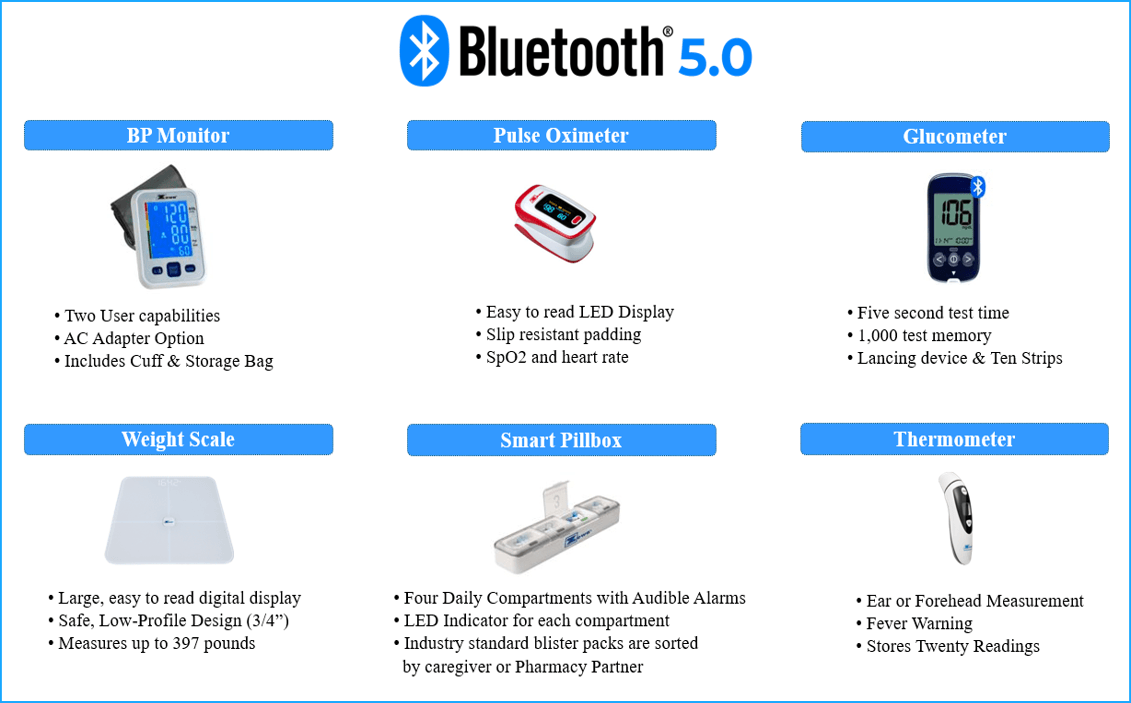
Our Bluetooth-connected device portfolio from Zewa Medical includes blood pressure monitors, glucose meters, digital thermometers, pulse oximeters, scales, and MedWell - an intelligent medication management pillbox.
Continuous health monitoring reduces the need for in-person visits, helping patients stay healthier at home while lowering healthcare costs.
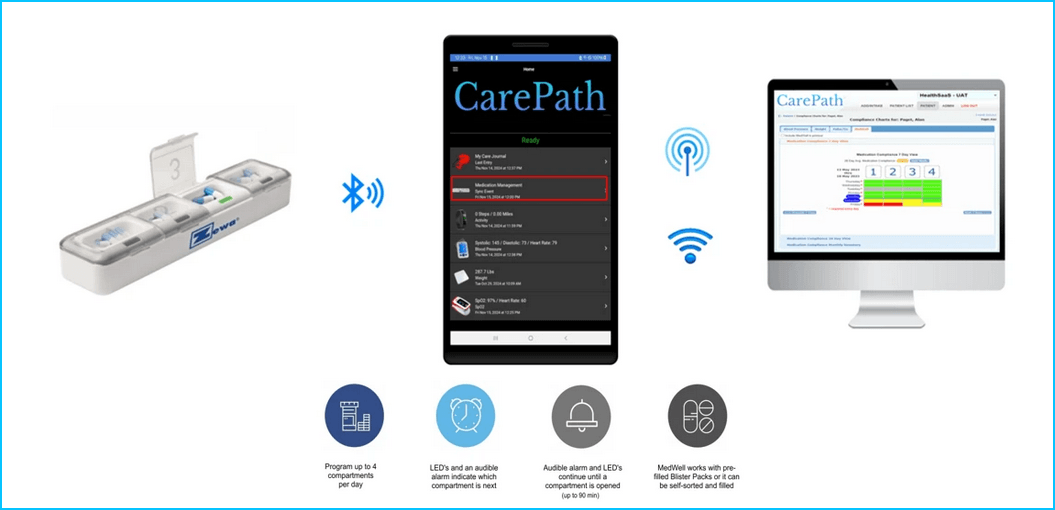
Medication Adherance
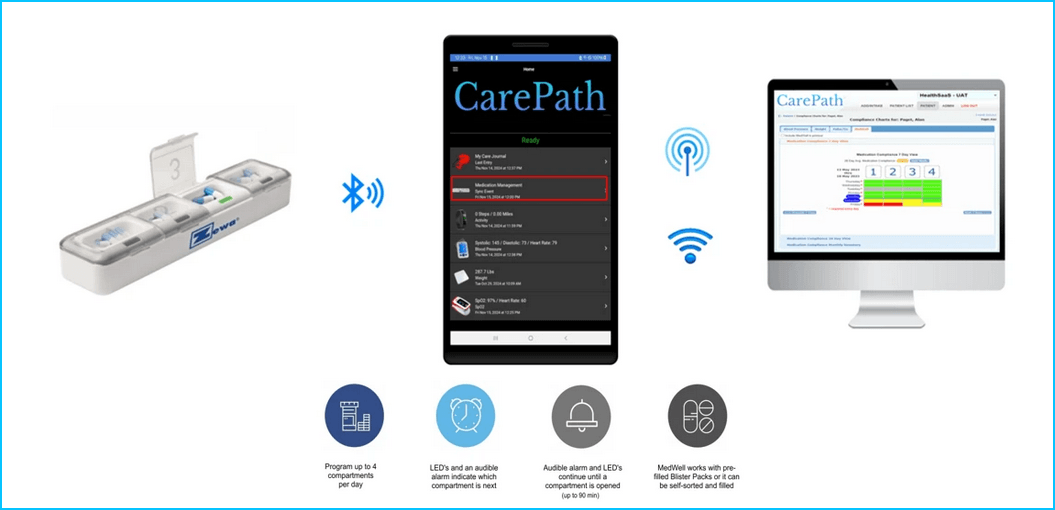
Navigating complex medication schedules presents a significant challenge for seniors striving to maintain theirindependence. Despite assistance from caregivers and family members, many struggle to follow their medication regimens consistently. A well organized approach is essential for preserving patients' autonomy while ensuring adherence to prescribed treatment plans.
Effective medication management requires educating both patients and caregivers about appropriate dosages, timing, and potential side effects. Comprehensive education, combined with clear communication protocols, helps seniors reduce the risk of medication errors or missed doses.
The MedWell Smart Pill Box represents an innovative connected health solution. The MedWell device features four compartments, each containing a blister pack for daily medications. An audible alarm and LED indicators alert users when it's time to access the correct compartment and take their medications. Data is sent to the CarePath mobile application and then routed to our Azure-hosted cloud portal, where clinicians can view adherence data in four unique chart views.
During the onboarding and ongoing wellness management program, Nurses will:
- Evaluate the individuals current medication plan.
- Provide medication reconciliation of both prescription and over-the-counter medications.
- Educate patients and/or caregivers on appropriate dosages, timing, and potential side effects.
- Track medication adherence and assess overall effectiveness.
The right medication at the righttime shouldn't be left to chance, it should be driven by intelligent technology and expert care.
Care Journals - Digital Questionniares

CarePath's digital questionnaires revolutionize patient-provider communication by delivering targeted, condition-specific assessments that capture critical clinical data often missed in traditional wellness monitoring solutions.
Enhanced Clinical Decision Making: Combining objective data and subjective feedback for our Ontological Knowledge System yields more accurate, comprehensive, and personalized evaluations, ultimately leading to improved treatment decisions.
Multi-Condition Early Warning Detection: Systematic symptom tracking across comorbidities identifies health deterioration patterns before crisis points
Comprehensive Quality of Life Assessment: Evaluation of how multiple treatments and conditions impact daily living, mobility, cognitive function, and psychological well-being.
Research-Based Intervention Protocols: Ontological Knowledge System assessments reference peer-reviewed medical literature, from complex comorbidity management to identify optimal timing and clinical interventions.
By integrating these advanced assessments into regular care routines, we promote a proactive approach to health management, enabling residents to participate in their health journeys actively. This personalized strategy not only enhances resident safety but also supports caregivers with the insights needed to address emerging health issues promptly, ultimately creating a holistic environment conducive to sustained wellness.
Personalized Care Plans

During the registration process, nurses develop individualized care plans tailored to address the specific health requirements of each individual, ensuring a comprehensive approach to wellness. These comprehensive plans provide actionable insights that foster proactive wellness management and enhance overall quality of life.
By combining medical history, device data, medication adherence monitoring and answers to user specific - digital health questionnaires we create actionable strategies that promote wellness and thriving in place.
US Based Virtual Nurses

By incorporating previous medical history, trending data from Bluetooth-enabled devices, digital health surveys, and medication adherence monitoring, our expert system generates detailed ontology assessments that onsite or US-based virtual nurses review.
Nurses use this information to identify patterns and trends, enabling the early detection of potential health concerns. This early detection of potential health concerns enables timely interventions, significantly reducing the risk of complications and hospitalizations.
Clinical Excellence
RADV - Risk Adjusted Diagnostic Validation
Clinical excellence begins with diagnostic accuracy. Risk Adjusted Diagnostic Validation (RADV) ensures therapeutic optimization is built on accurate diagnoses by leveraging independent AI-powered assessments against comprehensive clinical knowledge systems.Any attempt at therapeutic optimization begins with the correct diagnosisor diagnoses. RADV assessment is a process in which clinical data (including proposed primary and secondary diagnoses) are evaluated against an independent evaluation of the knowledge system in clinical decision support mode.
The process is iterative. If the system requires additional information for clarification,questions are returned for further consideration. The system then returns an appropriate differential diagnosis for consideration.
The report will either return a 'Reasonable' conclusion (when theindependent assessment supports the proposed diagnosis) or 'Conflicted' (when
other diagnoses may be a better fit for the data). Failure to address an RADV report deviating significantly from the diagnosis submitted will result in an automatic Suboptimal ORDS score. This ensures clinical assessments are built on accurate diagnostic foundations before any therapeutic recommendations are made.ORDS Scoring - The Therapeutic Optimization Framework
ORDS scoring is designed as a simple-to-understand reporting mechanism supported by an extensive evidence-based knowledge set that provides a transparent assessment of proposed clinical treatment plans. Unlike simple threshold-based notifications, which can lead to alert fatigue, our proprietary ORDS methodology systematically evaluates care patterns against peer-reviewed literature.
ORDS scoring is continuously updated to remain relevant as medicalknowledge evolves. Updating the scoring system is simple and does not require service interruptions. ORDS scoring also accounts for complex variationsrequired in patients with more than a single diagnosis.
The Ontological-Agentic AI system analyzes patient health profiles, medical history, and available lab and imaging data to compare proposed treatment plans with evidence-based medical literature and authoritative guidelines (e.g., the American Heart Association (AHA)). It returns an ORDS score with a complete rationale and supporting evidence. If additional data might affect final scoring, the system will present a series of questions for clarification.Additional questions might follow based on the received answers. The goal is to provide fully transparent assessment criteria based solely on therapeutic optimization in line with medical best practices.
Four-Level ORDS Classification:
Optimal: Care aligns perfectly with evidence-based best practices for the individual's specific profile
Reasonable: Care falls within acceptable clinical standards (particularly in situations without clear consensus)
Defensible: Care meets minimum acceptable standards based upon resource limitations
Suboptimal: Care patterns indicate significant deviations from literature recommendations.
Opportunities for alternative care plans are included with Suboptimal score reports
ORDS scoring is notfixed. Based upon outcomes analysis of operational data sets, the boundaries of
each class are expected to adjust over time.Applied Across Six Clinical Categories:
- Wellness and preventive care
- Health status and vital trends
- Prevention of disease progression
- Engagement and adherence
- Therapeutic optimization
- Quality of life metrics
The 3 R's Intervention Protocol: We deliver "the Right information, to the Right person, at the Right time" through intelligent triage. If one or more of the covered processes (prevention, diagnosis, disease management, medication adherence, engagement,etc.) are exhibiting suboptimal patterns, 3 R's triage is performed on each to determine the best care team member to engage and the appropriate timing of intervention triage to maximize efficient use of resources with the least disruption of routine workflow.
Triage Levels
- Emergent: Immediate referral to clinical backup
- Urgent: Response required within 24 hours
- Routine: Intervention scheduled within 5 business days
- Non-critical opportunities: Care enhancements added to monthly summary
This evidence-based classification and workflow system ensures your team receives nuanced, literature-backed clinical insights that consider the full complexity of each resident's situation, not just generic alerts. The ORDS framework solves the fundamental challenge facing Value-Based Care; it provides the quantifiable evidence and systematic workflow metrics necessary to demonstrate outcomes, justify interventions, and prove ROI.
Additional Details
Measurable Outcomes Through Continuous Quality Improvement(CQI):
Reduced hospital admissions through early intervention (critical for value-based arrangements)
- Improved medication adherence and therapeutic outcomes (better health at lower cost)
- Enhanced resident satisfaction and peace of mind (quality of life metrics matter)
- Operational predictability with fewer medical emergencies (sustainable operations)
- Competitive differentiation as a leader in proactive wellness management
- Continuous care quality improvement validated by third-party analysis
- Data-driven insights for ongoing service enhancement
- Documentation and evidence required for value-based care contracting
Our collaboration with the American Heart Association can provide participating client organizations with:
- Participation in groundbreaking outcomes research
- Access to cutting-edge cardiovascular health management protocols
- Third-party validation of care quality improvements
- Thought leadership positioning in the senior care industry
- The credibility and documentation needed for value-based care arrangements
- De-identified Outcomes Analysis: Ongoing outcome validation and CQI assessment, measuring
Clinical notification accuracy and appropriateness: - Care team performance metrics
- Identification of service enhancement opportunities
- Population health trends and intervention effectiveness
- The Force Multiplier Effect
- Technology-enhanced nursing model: 1000s of residents monitored simultaneously through automated data collection from Bluetooth-enabled devices (BP monitors, pulse oximeters, glucometers, weight scales, Smart pillbox & thermometers)
- AI-powered assessments combine objective device data with subjective digital questionnaire responses
- Intelligent triage notifications stratified by severity (Critical/Urgent/Routine/Informational)
- Literature-backed clinical rationale for every recommendation
- Focused care delivery where nurses receive prioritized alerts and can conduct personalized, informed interventions
Our Agentic AI - Ontological solution synthesizes resident health profiles, medical history, connected device data, and medication adherence data, combined with digital questionnaire responses. The system uses this information to deliver evidence-based clinical insights to nursing staff, supported by peer-reviewed medical literature, enabling precise risk stratification and appropriate care escalation.
Simplified Complex Care Management: Helps maintain independence longer by collecting data from Bluetooth-connected biometric devices, including Blood Pressure Monitors, Weight Scales, Pulse Oximeters, Glucometers, Body Temperature Thermometers, and a Bluetooth Smart Pill Box, with data analyzed by our Ontological Knowledge System provides nurses with actionable assessments that reference peer-reviewed medical literature
Reduced Hospital Visits: Through both consistent monitoring and profile-specific therapeutic optimization across multiple chronic conditions
Empowered Healthcare Participation: Comprehensive education about how medications work, why timing matters, and the health consequences of missed doses
Reduced Medication Errors: Intelligent systems explicitly designed for polypharmacy management and drug interaction preventionImproved Clinical Communication: Digital questionnaires help identify symptoms and concerns ross multiple conditions more effectively
Research-Backed Clinical Interventions: Leverage evidence-based protocols specific to complex comorbidity management to prevent health crises and optimize treatment effectiveness